Recently, the "Chinese Journal of Thoracic and Cardiovascular Surgery" published the "National Expert Consensus on the Management Strategy of Perioperative Perioperative Pulmonary Air Leak in Thoracic Surgery (2023)" in Volume 40, Issue 4, April 2024. This consensus fully explains the standardized diagnosis and treatment process and the consensus on the management strategy of persistent pulmonary air leak in preoperative evaluation, intraoperative operation and postoperative management, and provides recommendations.[1]
The consensus points out: "With the advancement of minimally invasive surgical technology and the popularization of the concept of accelerated recovery surgery, thoracic surgery is rapidly developing in the direction of minimally invasive and day-to-day surgery. However, patients after thoracic surgery are still at risk of postoperative complications. Among them, persistent pulmonary air leakage after surgery is still one of the most common complications of thoracic surgery. The incidence of persistent pulmonary air leakage is as high as 10% to 26%, which often troubles patients and medical staff. Persistent pulmonary air leakage has many adverse effects on patients, significantly prolonging the time of postoperative drainage and hospitalization, and may even cause serious complications, such as large-area subcutaneous emphysema, dyspnea, lung infection, incision infection, empyema, etc., which increase the mental and economic burden of patients and seriously affect their rehabilitation and the effective use of medical resources. Through the promotion and implementation of this consensus, it is expected to provide a more effective solution to the clinical challenge of persistent pulmonary air leakage, improve the diagnosis and treatment level of persistent pulmonary air leakage, promote patients to recover as soon as possible, shorten patients' hospitalization time, and provide strong support for the rapid recovery of patients after surgery."
For ease of reading, we organize the consensus content as follows:
Persistent pulmonary air leak is defined as pulmonary air leak lasting for more than 5 days.
(Recommendation level: 2A; expert agreement rate: 95%)
The high-risk population for persistent pulmonary air leakage should be evaluated before surgery, and preventive measures should be taken before, during, and after surgery to reduce the occurrence of persistent pulmonary air leakage. A history of chronic obstructive pulmonary disease and pleural adhesions are independent risk factors for persistent pulmonary air leakage.
(Recommendation level: 1B; expert agreement rate: 96%)
Surgical risk factors for persistent pulmonary air leakage include visceral pleural injury and rupture. It is recommended to use appropriate surgical techniques to minimize or avoid visceral pleural rupture. When patients with high-risk factors such as COPD or emphysema undergo pulmonary surgery, they can use thoracic surgical biological patches with relevant indications to prevent pulmonary air leakage in a standardized manner after preoperative evaluation. .
(Recommendation level: 1B; expert agreement rate: 97%)
At the end of lung surgery, it is recommended to evaluate the degree of lung leakage, preferably by immersion test; the insufflation pressure is recommended to be controlled at 20~30cmH2O.
(Recommendation level: 2A; expert agreement rate: 92%)
If pulmonary leakage is detected during surgery, mild leakage can be left untreated, and moderate to severe leakage is recommended to be actively treated during surgery; conventional mechanical methods such as surgical suturing or cutting closure are preferred; when conventional methods are still unsatisfactory, it is recommended to use high-tech materials such as medical adhesives with indications to prevent pulmonary leakage.
(Recommendation level: 2A; expert agreement rate: 92%)
The type, number, position and side hole of the chest drainage tube are very important for the treatment of patients with pulmonary air leakage. The number and type of drainage tubes can be reasonably selected according to the specific situation during the operation. For moderate to severe air leakage, it is recommended to leave a conventional thick tube.
(Recommendation level: 2A; expert agreement rate: 92%)
Negative pressure suction has clinical application value for patients with persistent pulmonary air leakage, and it is necessary to select the appropriate negative pressure drainage method according to the specific situation.
(Recommendation level: 2B; expert agreement rate: 89%)
Digital chest drainage system can be used to treat persistent pulmonary air leakage. Its retrospective air leakage curve provides physicians with a more objective clinical basis for adjusting the negative pressure suction value, which helps to shorten the drainage time and hospitalization time.
(Recommendation level: 2B; expert agreement rate: 88%)
Pleurodesis is an important clinical method for treating persistent pulmonary air leakage, which can alleviate the degree of pulmonary air leakage and shorten the duration. The type of drug can be reasonably selected according to the specific situation.
(Recommendation level: 2A; expert agreement rate: 90%)
For patients with persistent pulmonary air leakage, if they meet specific conditions, a professional medical team can perform home digital chest tube management, which can effectively manage the patient without increasing related complications or mortality, ensuring the patient's safety and efficacy. (Recommendation level: Level 3; Expert agreement rate: 82%)
Patients with persistent pulmonary air leakage (especially bronchopleural fistula) who cannot be resolved by conservative treatment may consider surgical treatment or endoscopic interventional treatment, but a multidisciplinary discussion should be conducted to develop an individualized treatment plan based on the patient's specific situation.
(Recommendation level: 2A; expert agreement rate: 90%)
The content above are the key points of the National Expert Consensus on Management Strategies for Perioperative(2023)
It is worth noting that this consensus 3 clearly states: "Surgical risk factors for persistent pulmonary air leakage include visceral pleural injury and rupture. It is recommended to use appropriate surgical techniques to minimize or avoid visceral pleural rupture. When patients with high-risk factors such as COPD or emphysema undergo lung surgery, they can use thoracic surgical biological patches with relevant indications to prevent pulmonary air leakage in a standardized manner after preoperative evaluation. (Recommendation level: 1B; expert agreement rate: 97%)"
Non-cross-linked porcine small intestinal submucosa (SIS) extracellular matrix material is currently an ideal reinforced surgical biological patch material for solving persistent pulmonary air leakage (PAL) after lung resection and shortening patients' postoperative hospitalization time. James R. et al. proposed an innovative method called "Standardized Postoperative Air Leak Reduction (STAR)", which includes three factors related to air leakage reduction: fissureless operative technique, staple line buttressing, and protocol-driven chest tube management. The study analyzed 475 patients who underwent lung resection using STAR (264 lobectomies, 198 wedge resections, and 13 segmentectomies) [2]. All patients used SIS material biological patches to reinforce the anastomosis during surgery. The results were compared with the data from the National Database of the Society of Thoracic Surgeons (2012-2014). The results showed that the STAR method combined with SIS material biological patches to reinforce the lung anastomosis could reduce the incidence of PAL after lobectomy by 52% (5.7% vs. 10.9%, P=0.0079) and the incidence of PAL after wedge resection by 40% (2.5% vs. The results showed that the SIS material biological patch can reduce the effectiveness of postoperative pulmonary air leakage, and its combination with STAR can bring more benefits to patients.
Surgical method | Number of cases | PAL incidence (using STAR technology) | PAL incidence (routine) | Reduction rate | P-value | Length of hospital stay (days/using STAR technology) | Hospital stay (days/routine) | P-value |
Lobectomy | 264 | 5.7% | 10.9% | 52% | P=0.0079 | 3.2 | 6.3 | P=0.0001 |
Wedge resection of lung | 198 | 2.5% | 4.2% | 40% | P=0.3841 | 3.3 | 4.5 | P=0.0152 |
Segmental resection of lung | 13 | 7.7% | 7.4% | - | P=0.2292 | 3.2 | 5.2 | P=0.0001 |
Clinical benefits of STAR combined with SIS material biological patch on PAL incidence and hospital stay
As the experience of STAR technology in clinical application accumulated, the team members further analyzed the effect of STAR technology combined with SIS material biological patch on the postoperative hospitalization time of 390 patients undergoing lung resection [3]. The results showed that since the use of STAR technology in 2010, the average postoperative hospitalization time of patients was 3.9 days, and 38% (240 cases) of patients could be discharged on the first day after surgery (POD1); and the postoperative hospitalization time was shortened year by year with the application of STAR technology combined with SIS material biological patch. In 2017, about 63% of patients could be discharged on POD1 (Figure 3). In addition, postoperative patient satisfaction increased significantly, hospitalization costs decreased, and the patient's readmission rate, complication incidence or mortality rate within 30 days were not increased. This result further confirmed the effectiveness and safety of STAR technology combined with SIS material biological patch in shortening patient hospitalization time.
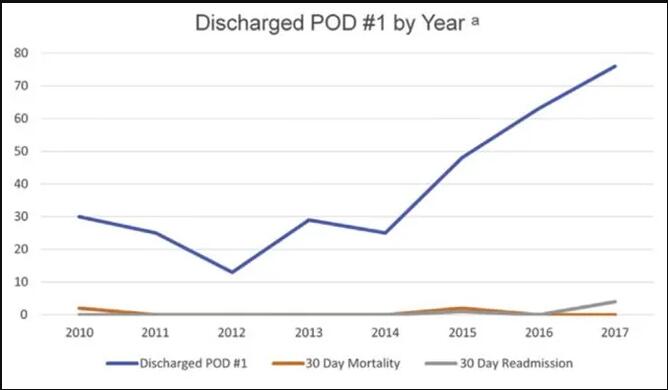
Figure 1 Clinical benefit of STAR combined with SIS material biological patch on postoperative hospital stay
One of the reasons why SIS material biological patches can effectively reduce postoperative lung leakage in lung resection patients is that SIS materials can provide better pressure resistance for lung anastomosis. The results of an animal experiment conducted in a pig lung model showed [4] that compared with reinforced patch materials such as synthetic (PGA, ePTFE) and bovine pericardium, lung anastomosis reinforced with SIS material biological patches showed a higher leakage threshold (SIS vs. PGA vs. ePTFE vs. BP: 75 vs. 40 vs. 20 vs. 40 cmH2O, Figure 4), indicating that the material can effectively seal the lung anastomosis at higher airway pressures, exert better pressure resistance, and prevent lung leakage.
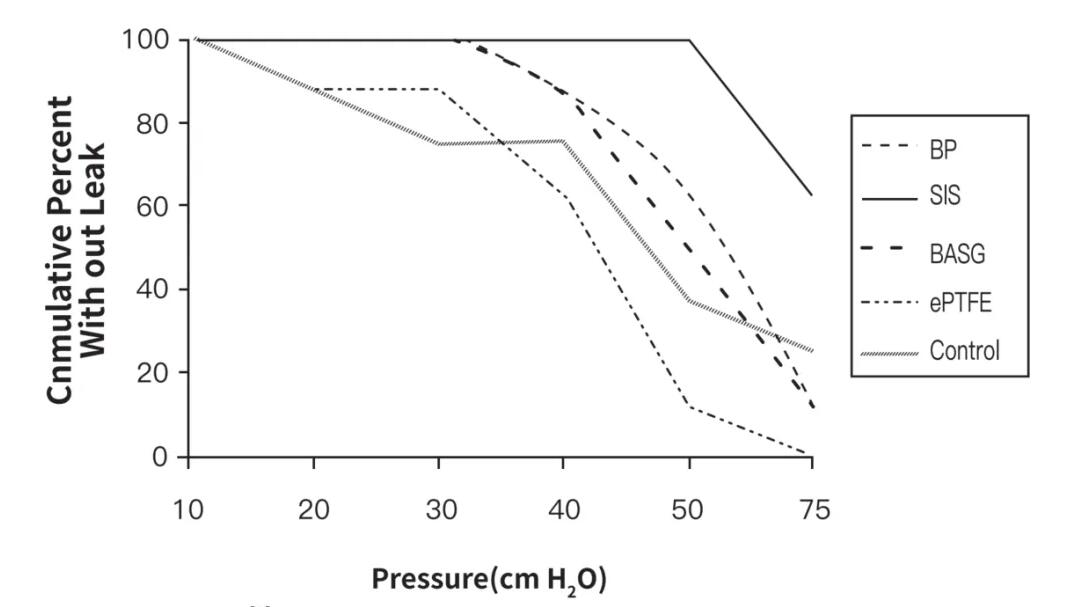
Figure 2 Compression performance of SIS material biological patch for lung anastomosis reinforcement
The domestic innovative product - Borriqiang® Anastomotic Reinforcement Patch (Figure 3) is made of non-cross-linked, highly bioactive, decellularized SIS extracellular matrix (ECM) as raw materials. It is used with a stapler and is stably fixed at the anastomosis during the firing process of the stapler. It can evenly disperse the stress of the staples on the lung tissue and reduce the cutting damage to the lung tissue by the staples. It realizes the functions of reinforcement, hemostasis, and air leakage prevention, and effectively avoids the problems of anastomotic leakage and bleeding in traditional stapler surgery (Figure 4).
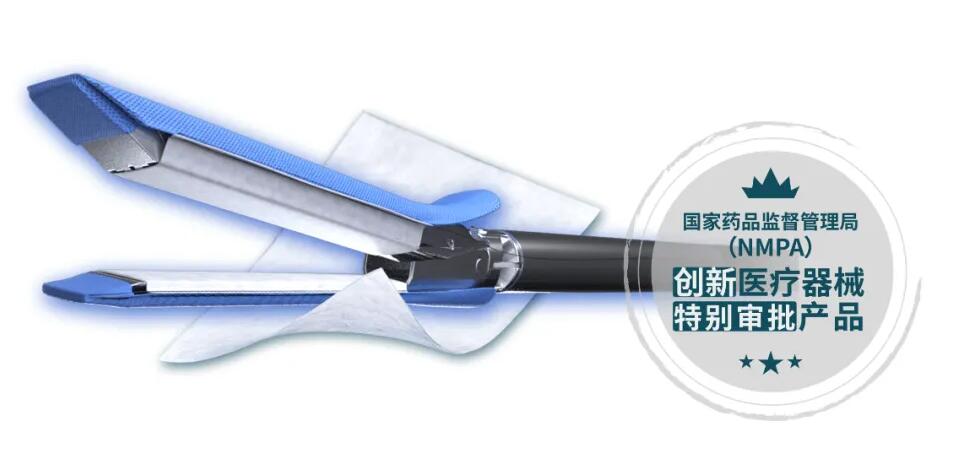
Figure 3 Schematic diagram of the Borrqiang® Vidasis SIS Stapleline Reinforcement product
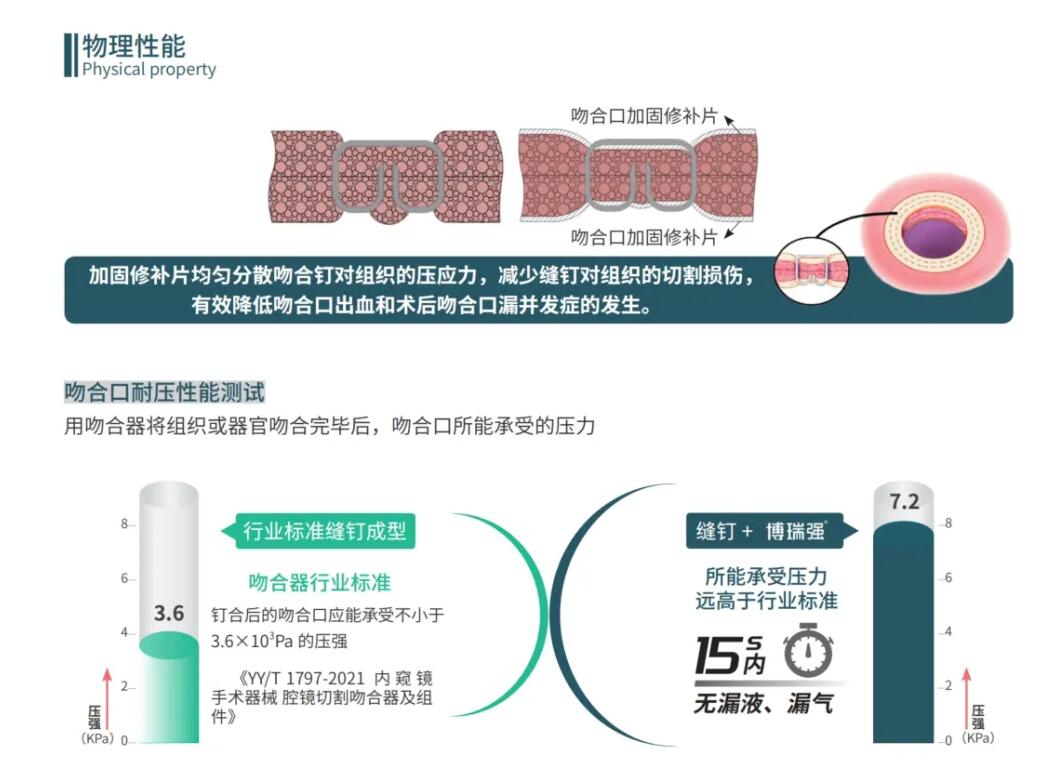
Figure 4 Schematic diagram of the working principle of the Borrqiang® Vidasis SIS Stapleline Reinforcement product
Borriqiang® Anastomotic Reinforcement Patch has the following advantages (Figure 5):
1) The SIS material processed by non-cross-linking process retains the complete three-dimensional structure of ECM, and is rich in multiple bioactive factors, which can quickly vascularize and induce tissue regeneration and repair, and can be completely degraded [5, 6], without any foreign matter residue, and has excellent anti-adhesion properties [7];
2) Secondly, compared with synthetic materials, SIS material has better biocompatibility, avoiding the foreign body reaction and secondary fiber wrapping and chronic inflammatory reaction caused by synthetic materials [6, 8];
3) In terms of anastomosis assembly performance, the innovative fixation design is adopted, so that the product can be tightly fixed to the anastomosis device without the use of adhesives, and can be used with a full range of anastomosis devices, ensuring the versatility of the product.
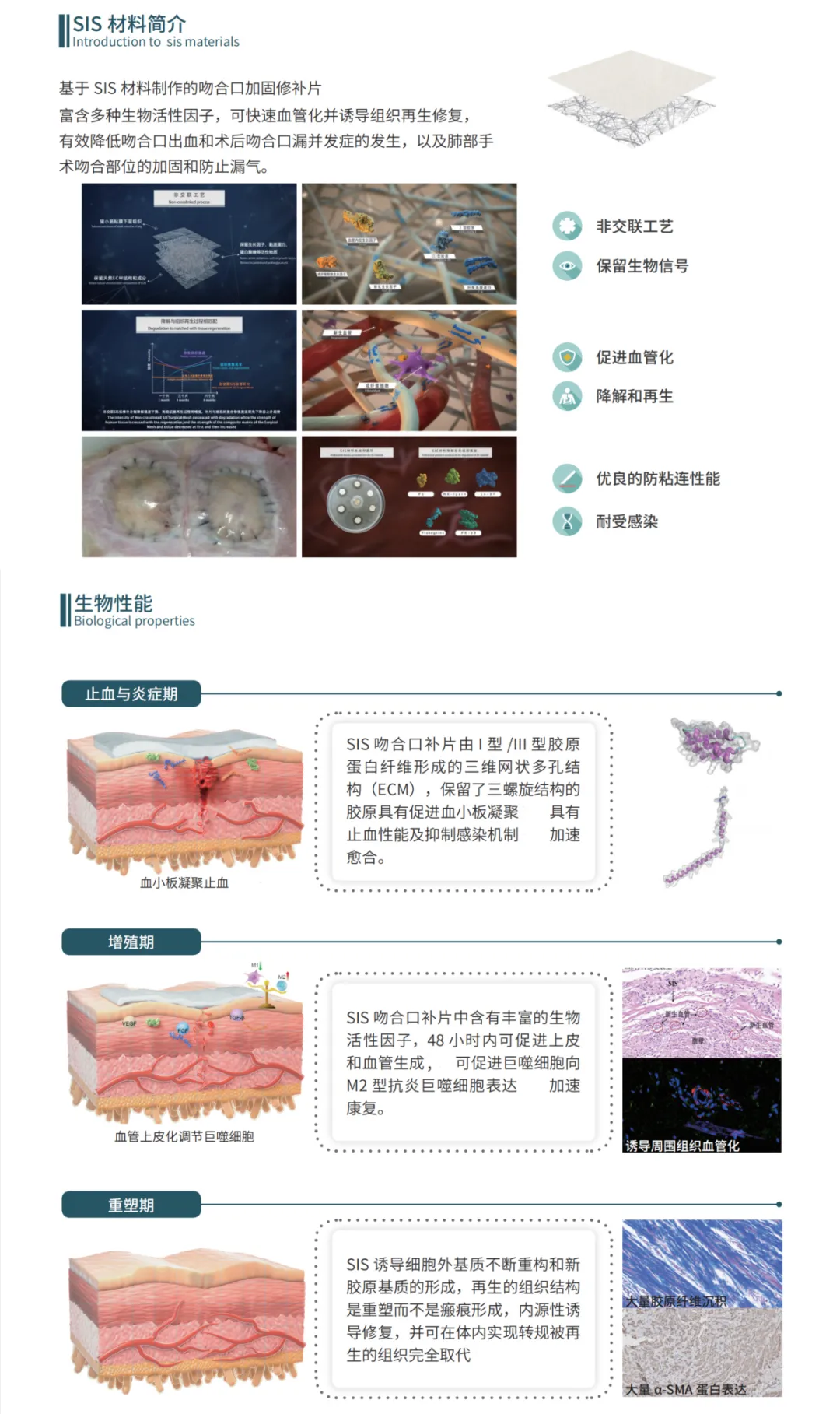
Figure 5 Product advantages and mechanism of Borrqiang® Vidasis SIS Stapleline Reinforcement
As an innovative medical device approved by the National Medical Products Administration, BIOSIS HEALING Borriqiang® Anastomotic Reinforcement Patch is suitable for gastrointestinal surgery, colorectal anal surgery and other digestive tract surgeries in addition to its application in lung surgery. Since obtaining the certification in August 2022, it has been widely used in clinical practice and has been recognized by clinicians at home and abroad. We believe that with the continuous popularization of clinical applications, the domestic innovative product Borriqiang® Anastomotic Reinforcement Patch will provide a more effective solution to the clinical challenge of persistent pulmonary air leakage, promote patients to recover as soon as possible, shorten their hospital stay, provide strong support for patients to achieve rapid recovery after surgery, and benefit more patients.
[1] Chinese Medical Association Thoracic Surgery Branch, Wu Jieping Medical Foundation Lung Cancer Professional Committee, Chinese Anti-Cancer Association Lung Cancer Integrated Rehabilitation Professional Committee, etc. National expert consensus on management strategies for persistent pulmonary air leak during perioperative thoracic surgery (2023)[J]. Chinese Journal of Thoracic and Cardiovascular Surgery, 2024, 40(04): 193-200.
[2] Drahush N, Miller AD, Smith JS, Royer AM, Spiva M, Headrick JR Jr. Standardized Approach to Prolonged Air Leak Reduction After Pulmonary Resection. Ann Thorac Surg. 2016 Jun;101(6):2097-101.
[3] Greer S, Miller A D, Smith J S, et al. Safety of Next Day Discharge After Lobectomy: Have We Broken the Speed Limit?[J]. Ann Thorac Surg, 2018,106(4):998-1001.
[4]Downey DM, Harre JG, Pratt JW. Functional comparison of staple line reinforcements in lung resection. Ann Thorac Surg. 2006 Nov;82(5):1880-3.
[4] Zhao P, Li X, Fang Q, et al. Surface modification of small intestine submucosa in tissue engineering. Regen Biomater. 2020;7(4):339-348.
[6]Cao G, He W, Fan Y, Li X. Exploring the match between the degradation of the ECM-based composites and tissue remodeling in a full-thickness abdominal wall defect model. Biomater Sci. 2021;9(23):7895-7910.
[7]Liu C, Pei M, Li Q, Zhang Y. Decellularized extracellular matrix mediates tissue construction and regeneration. Front Med. 2022;16(1):56-82.
[8]Lin X, Wang W, Zhang W, et al. Hyaluronic Acid Coating Enhances Biocompatibility of Nonwoven PGA Scaffold and Cartilage Formation. Tissue Eng Part C Methods. 2017;23(2):86-97.